Community-based Kidney Medicine & Preventive Nephrology©
Understanding Perspectives of Chronic Kidney Disease at Community & Undertaking Preventive Nephrology at Core
_____________________________________
Contents
1. Community-based Kidney Medicine - basic education
2. CKD Education at Community - risks for development of CKD
3. Preventive Nephrology - once you develop CKD, what do you need to do to prevent progression
4. How to select CKD friendly food
5. Pandemic and CKD
6. how to lower creatinine levels fast
8. References:
CKD Initiative vocal presentation
===================
1. Community-based Kidney Medicine - basic education
- Chronic Kidney Disease (CKD) - Renal perspectives at community
- Concepts of Renal Failure as a Preventable Disease
- Concept of CKD at Zero level (CKD-0)
- Role of GP at Primary Health Clinics
- Role of APN (Advanced Practising Nurse) at Primary Health Clinics
- Role of renal residents at community level
2. CKD Education at Community - risks for development of CKD
- How could GP know if patient's Kidney is at CKD risk
- What do GP need to do - to prevent development of CKD
- Councelling by Renal APN Nurse - Patient Education to minimise initiation of CKD
3. Preventive Nephrology - once you develop CKD, what do you need to do to prevent progression to dialysis requiring stage; you need to attend to the followings:
- HALT CKD- How to retard
- STOP CKD- How to control
- PROTECT CKD- from AKI, How to
- TREAT CKD- How to
- PLAN RRT- How to
- LEARN CKD- more about CKD education from expert
4. How To Select CKD Friendly Food - to avoid food rich in nephrotoxic substances: i.e.
- Oxalate - leads to rapid deterioration of CKD
- Potassium - leads to cardiac arrest in CKD
- Phosphate - leads to renal bone disease in CKD
- Uric acid - leads to progression of CKD
- Salt - increases blood pressure in CKD
- Fat - responsible for stroke and heart attack
- Protein - responsible for CKD progression.
5. Pandemic and CKD: Patients Role - what need to be done
__________________________________
__________________________________
1. Community-based Kidney Medicine - basic education
The basic education involves the following topics:
- Renal perspectives at community: in developed countries, 11% of population have any stage of CKD. In developing countries the rate is possibly higher. That means one of nine people at any community, may have CKD in the absence of people knowing it. As such, people become aware of CKD only in advanced stages when CKD retardation becomes difficult.
- Renal Failure is Preventable: Therfore, CKD anticipation at early levels is the PRIMA FACIE of the Concepts of Renal Failure is Preventable Disease. After initial start, CKD progress happens as a vicious cycle of advancement because of multitudes of avoidable external insults. That is why CKD anticipation should start before CKD development. I used the term CKD-0 for this stage.
- Concept of CKD at Zero level (CKD-0): Therefore detecting CKD at the bud is the key to prevention.
- Role of GP at Primary Health Clinics is the game changing step for identification of CKD-0 and asymptotic CKD stages.
- Role of APN (Advanced Practising Nurse) at Primary Health Clinics would start subsequently according to me for protocolised Preventive approach, as described by me (also available in my public web-edu site, renalfailureadvice. com) below.
________________________________
2. CKD Education at community - risks for development of CKD.
CKD in community - how to detect?
The basic strategy is as follows:
- How GP knows if patient's Kidney is at CKD risk? Patients with Hypertension, Diabetes Mellitus, Cardiovascular disease, Structural renal tract disease, renal calculi or prostatic hypertrophy, Multisystem diseases with potential kidney involvement – for example, SLE, Family history of CKD or hereditary kidney disease, Haematuria and proteinuria.
- GP need to do according to NHS - UK guidelines - CKD testing to these peoples. with the following risk factors:
CKD testing at community level:
- UFEME and UPCR.
- UECr and eGFR.
- Monitor eGFR in people prescribed nephrotoxic drugs.
- Check eGFR at least annually in people receiving long-term systemic NSAIDs.
- US Doppler kidney when indicated.
Look for progression factors for CKD:
Potentially reversible aggravating factors:
- Salt and water depletion - dehydration
- Systemic or renal infection
- Accelerated hypertension
- Use of Nephrotoxic drugs
- Urinary tract obstruction
- Acute heart failure
- Hypercalcaemia
Councelling by Renal APN Nurse - Patient Education to minimise initiation of CKD
Reinforcing the above and highlighting the below:
- Incidence of CKD in the Community of the world
- Incidence of ESRF (End Stage Renal Failure) and decline of eGFR
- Causes of CKD in the community
Decline of eGFR, and incidence of ESRD. The rapid decline from any kidney injury, leads to early ESRD. lnjuries affect each renal components in a vicious cycle hastening renal death.
Addressing the Intiating Factors. Together with standard therapy with RAAS inhibitors. In cases of GN. Maintenance of low dose immunosuppressive, as prescribed, in long term basis.
__________________________ 3. Preventive Nephrology - community based approach to prevent CKD progression
Community-based Kidney disease education, knowledge of CKD, prevention of CKD progression by renal doctor and renal advanced practicing nurses in the following apects:
DETECTING CKD
STOP CKD- How to control
HALT CKD- How to retard
PROTECT CKD- from AKI,
How to TREAT CKD-
How to PLAN RRT-
How to LEARN CKD- more about CKD education from experts
_____________________________________
DETECTING CKD
☑ Calculate your CKD risk scores at UK NHS Qkidney risk calculator©.
☑ Check urine routine test & Protein/Creatinine ratio.
☑ Do blood tests for glucose and Creatinine.
☑ Check your Blood pressure.
☑ Do ultrasound of kidney.
With all results, visit a kidney specialist.
Keeping surveillance
Repeat the blood & urine tests 🗒every 2/3 years with advise of the doctor.
__________________________________
STOP CKD
How do you stop CKD progression
Retarding CKD progression.
CKD progresses over the years with reduction of eGFR by more than 4% every year. You can retard this progression by careful lifestyle and food habit as follows:
🛑 Minimize eating fruits and vegetables not so good for kidney disease.
🛑 Minimize eating mushroom 🍄 fresh or dry.
🛑 Minimize eating red meat 🍖 and raw seafood.
🛑 Minimize eating fastfood and food with too much salt and gravy from foodstalls.
🛑 Stop eating health supplements and traditional medicines without consulting a kidney specialist.
🛑 Minimize eating all kinds of preserved food and shelffood.
🛑 Stop drinking / eating fruit and vegetable concentrates.
🛑 Stop getting dry by too much running, 🏃 jogging, and exercise.
🛑 Stop smoking 🚬 and drinking.
_________________________________
HALT CKD
How do you control CKD to halt it?
Once you have been diagnosed with CKD, be reminded that it is progressive like a plane ✈ on the runway track. You need to halt its progression by taking control of all relevant parameters as follows:
🎮 Control high blood pressure, try to keep less than 140/90 mmHg (130/80 if you have protein leak in urine). This matters - not the number of 💊 you take.
🎮 Control diabetes, HbA1C less than 7%.
🎮 Control nephritis by continuing some immunosuppressive medicines given by your kidney specialist regularly.
🎮 Control urine protein as low as possible, at least less than 1 by maximising ACEI / ARB / MRA, and eating less protein.
🎮 Control BMI to less than 25 by eating less fatty /oily /calorie rich food.
🎮 Control water overload by moderating water intake.
🎮 Control blood cholesterol by diet check and medicine.
🎮 Do not get heart attack, control your heart by medicines and diet.
🎮 Control lifestyle, do not get urine infection frequently.
_____________________________________
PROTECT CKD
Protect your Kidney from AKI (Acute Kidney Injury) to prevent CKD worsening.
Acute Kidney Injury (AKI) on CKD
Each time an episode of acute Kidney Injury happens on your CKD state, your CKD worsens and progresses to next stage.
Avoid getting Acute Kidney Injury frequently by protecting yourself from the following situations:
⚠ Vomiting / diarrhoea / dehydration.
⚠ Too high / too low BP.
⚠ Flu / fever / infection / sepsis.
⚠ Body injuries / accidents / surgery / anesthesia.
⚠ CT scan with contrast.
⚠ Poisoning / toxin / toxic antibiotic.
⚠ Pain gel / plaster / NSAID 💊.
⚠ Kidney stones.
⚠ Heart attack.
⚠ Too much 💦 water & salt intake.
⚠ Liver virus by taking vaccine. against hepatitis B virus.
⚠ Frequent dehydration during air travel and holidays.
⚠ Traditional medicines.
_____________________________________
TREAT CKD
How do you treat CKD
Meticulously comply with doctor's treatment with regular followup. Treatment & Compliance in CKD.
Other than making urine, your Kidney has many important functions. Failing kidney cannot perform its many kinds of Jobs, it needs help to make up with these deficiencies.
The following statements will help you understand, and you will be able to follow instructions accordingly:
😣 Take less salt (5gm/day) and required amount of water.
😣 Take Lasix 💊 to get rid of excess water by consulting kidney specialist.
😣 Keep your weight stable (BMI<25).
😣 Check BP at home, keep it within limits.
😣 Check glucose before meals weekly, keep it <7
😣 Visit dietician,
⚠ Minimize fruits / vegetables rich in potassium (<2g/day), phosphate (<0.8g/day), oxalate (<0.2g/day) and protein (<0.8g/kg/day).
😣 Keep hemoglobin (Hb) 11-12g/dl, take iron pills💊, If needed get Erythropoietin injection 💉 prescribed by kidney specialist.
😣 Take vitamin supplements and Calcium 💊 with food. You may also need active Vit D.
😣 Take ACEI / ARB / MRA according to doctor's advise.
😣 Vaccinate💉 yourself against influenza, pneumonia and Hepatitis B virus.
😣 Check blood urea, sodium, potassium, bicarbonate, creatinine, glucose, cholesterol, calcium, phosphate , iPTH, Hb and eGFR every 2-6 months depending on your Kidney doctor's advice.
😣 Do not forget your heart and liver conditions.
😣 Remember to bring your medicines for doctors to check during your follow up appointment.
_____________________________________
PLAN RRT
Plan longterm Renal Replacement therapy early, keep calm and carry on.
Plan longterm RRT early, keep calm and carry on.
Plan early for RRT.
May be after 5, 10, 20 years (or never) kidney stops functioning needing you to get RRT for survival. You can make plan early for renal replacement therapy (RRT) which could be haemodialysis, peritoneal dialysis and kidney transplant. The following will help you to get assistance:
⚒ Get your ACP (advance care plan) ready. Approach MSW (medical social service).
⚒ Decide for future dialysis/transplant when Creatinine worsens to 400 umol/L (4.6 mg/dL) as per your Kidney doctors advice. Talk to RC (renal coordinator).
⚒ Get AVF (AV fistula) done for haemodialysis. Visit VS (vascular surgeon).
⚒ Or get TK catheter when Cr further worsens to 600 umol/L (7 mg/dl) for peritoneal dialysis.
⚒ Or get a donor for transplant this time. Visit TC (transplant coordinator).
⚒ Do not lag behind.
__________________________________
References
learning more about CKD from the web
The following websites are for public education on CKD. You might find them useful. The advices in this CKD advice website is in conformity with them. You are encouraged to visit these links.
1. NHS UK, Chronic kidney disease education.
2. Mayo clinic, kidney self-management.
3. Cleveland Clinic, food and kidney.
4. Pro inflammatory diet that harms CKD.
5. Central level measure in Japan for CKD prevention and returdation.
_________________________________
4. How To Select CKD Friendly Food - to avoid food rich in nephrotoxic substances: i.e.
- Oxalate - leads to rapid deterioration of CKD
- Potassium - leads to cardiac arrest in CKD
- Phosphate - leads to renal bone disease in CKD
- Uric acid - leads to progression of CKD
- Salt - increases blood pressure in CKD
- Fat - responsible for stroke and heart attack
- Protein - responsible for CKD progression.
GOOD FOOD HABITS: FOOD TO AVOID IN CKD TO RETARD PROGRESSION AND OTHER INJURIES
Food to avoid in CKD.
Avoid the highlighted zones.Good food habit in CKD.
Food habit is very important in CKD.
Certain food can be life threatening, some food may affect Skeleton growth, some food can affect metabolic syndrome, some food may cause vascular damage, while some kind of food may cause acute Kidney injuries (AKI) and some food may cause rapid worsening of CKD.
Therfore, you need to be mindful of what you eat.
Certain food, fruits and beverages are high in potassium content. Consuming these in unrestricted amount in CKD may lead to high blood lebel as CKD kidney cannot remove. This causes lkfe threatening heart rhythm and carfiac arrest and death.
Calcium, Phosphate and vitamin D are regulated by normal kidney. CKD state causes disregulation leading to bone disorders. In CKD, phksphate level increases as kidney cannot remove it from blood. These food, highlighted red, are high in Phophate, ao should be restricted
____________________________ 5. Pandemic and CKD, what you need to care about? (A) Guidance for CKD, (B) Current Therapy, (C) Vaccines.
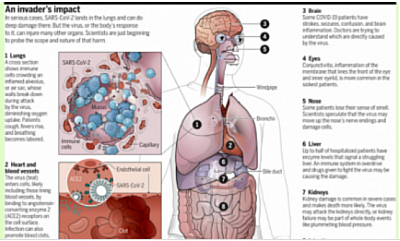
PANDEMIC, as a Chronic Kidney Disease patient, what should you do. Coronavirus (COVID-19) guidance for patients with kidney disease
A) Coronavirus (COVID-19) guidance for patients with kidney disease.
- Some information on COVID-19: Incubation period and infection.
- These advices have been produced by the Kidney Care organizations of UK for chronic kidney disease patients during the perid of COVID-19 pandemic.
- Please go to the link below to get your desired information.
https://www.kidneycareuk.org/news-and-campaigns/coronavirus-advice/
Covid-19 in CKD
Abridged from the above website.
* a new continuous cough
* Then self-isolate and stay at home for seven days if you live alone and you and your whole household should stay at home for 14 days if you share a home with other people.
* Please do not go to your renal unit until you have spoken to them on the telephone,
* and do not go to your GP or pharmacy.
* Dialysis patients with symptoms of COVID-19 should contact their dialysis unit and the dialysis unit can then ensure that kidney care continues to be provided.
* Please don't go directly into your unit until you know what arrangements are being made for you.
* If you have had a transplant and believe you have COVID-19 you should let your transplant unit know. You are now being advised to self-isolate for 12 weeks regardless of having symptoms.
* Do not visit the GP or pharmacy
* Do not chnge your medications unless advised to do so by your renal unit.
* Do not leave your house.
* Do not attend any gatherings. These include gatherings of friends and families in private spaces for example family homes, weddings and religious services.
* Do not go out for shopping, leisure or travel and, when arranging food or medication deliveries, these should be left at the door to minimise contact.*
* Keep in touch using remote technology such as phone, internet, and social media.
2. If you're a contact of a COVID-19 case, or
If you are in Lock Down area,
then stay home.
Stay at Home
* Only go outside for food, health reasons or work (but only if you cannot work from home)
* If you go out, stay 2 metres (6ft) away from other people at all times
* Wash your hands as soon as you get home
* Do not meet others, even friends or family.
* You can spread the virus even if you don’t have symptoms.
3. People who have had a transplant or take a certain level of immunosuppressive medicines are advised to start strict self-isolation.
Basic science Other group of patients that need self-isolation
You are at very high risk and will need to self-isolate yourself if you are in at least one of the following groups:
* You have a transplant
* If you over 70 and are on any form of immunosuppression or have been on one in the past
* Your kidney disease is caused by inflammation, a condition of your kidneys (sometimes called an autoimmune condition) AND-
* If you are currently receiving intravenous cyclophosphamide treatment or rituximab treatment or have done so within the last 6 months
* If you are receiving cyclophosphamide treatment as tablets (oral treatment)
* If you have received prednisolone at a dose equal to or above 20mg tablets every day for more than 4 weeks any time within the last 6 months
* If you have received or currently are receiving more than 5mg every day of prednisolone for greater than 4 weeks taken with at least one other immunosuppressive type of medicine within the last 6 months.
* If you suffer with nephrotic syndrome
* For children, who have the above kidney diseases.
__________________________________
B) Current strategies against Corona Virus
1. Approved latest antiviral treatment for Covid-19 Molnupiravir: First oral agent (Generic by BAXIMCO and Original by MSD)
2. IL-6(R) mab: (targeting CRS that happens in SIRS)
3. Anti-viral Remdesivir (Ebola agent)
4. Convalescent plasma (donates plasma of recoverwd pt): (Blocking antibidy)
5. Autologus stem cell inhalation: (repopulating pneumocytes)
6. Antiarthritis medicine, (anti-inflammatory medicine)
World Health Organization panel had earlier this year recommended baricitinib for patients with severe COVID-19 in combination with corticosteroids.
Baricitinib belongs to a class of drugs called Janus Kinase (JAK) inhibitors which work by blocking actions of enzymes that play a role in the immune system processes and lead to inflammation, often seen in severe COVID-19 as lung damage.
In the RECOVERY trial, baricitinib also increased the chances of patients being discharged alive within 28 days and reduced the risk of their condition worsening, scientists said.
Scientists behind the RECOVERY trial had shown dexamethasone saved the lives of COVID-19 patients, in what was called a "major breakthrough" in the pandemic, and also found tocilizumab worked against coronavirus.
Drug:
Molnupiravir works by disrupting the virus’s reproduction.
Once the virus gets inside the body’s cells, it replicates its genome, which is made not of DNA but RNA (ribonucleic acid). These replicated genomes are then formed into complete virus particles which burst out of the cell and continue to spread around the body.
However, the molecules of molnupiravir are absorbed by virus-infected cells, where they are converted into a defective version of the building blocks of RNA. So, when the virus tries to replicate, the resulting virus particles have defective genetic material and can no longer reproduce. This means that the viral load should remain low, which reduces the risk of serious disease.
Since molnupiravir targets the RNA that SARS-CoV-2 uses as its building blocks, it should be equally effective against all coronavirus variants.
“This mechanism of action has some limitations and the drug cannot be given to pregnant women due to the risk of damaging an unborn baby,” said Prof Penny Ward, Visiting Professor in Pharmaceutical Medicine at King’s College London.
------------------------
6. Vaccine:
https://www.channelnewsasia.com/news/world/coronavirus-covid-19-uk-vaccine-doses-12695182
7. But everything down to maintaining clean status.
____________________________________
C. Vaccines for COVID-19
COVID-19 Vaccines
Pfizer & Moderna vac: It is an RNA vaccine composed of nucleoside-modified mRNA (modRNA) encoding a mutated form of the spike protein of SARS-CoV-2, which is encapsulated in lipid nanoparticles. The vaccination requires two doses given three weeks apart. The particle fuses with cells and with cellular protein synthesis to produce the spike protein. This spike proteins induces antibody production by T lymphocytes against the corona virus spike protein to provide the immunity.
Oxford-Sputnik vac: A diagram showing how the Oxford COVID-19 vaccine works. A chimpanzee adenovirus is used in the ChAdOx1 viral vector, engineered to match the SARS-CoV-2 spike protein. The Oxford vaccine contains the genetic sequence of this surface spike protein. When the vaccine enters cells inside the body, it uses this genetic code to produce the surface spike protein of the coronavirus. This induces an immune response, priming the immune system to attack the coronavirus if it later infects the body.
Sinovac or CoronaVac: Chinese vaccine is an inactivated vaccine candidate against COVID-19, created from African green monkey kidney cells (Vero cells) that have been inoculated with SARS-CoV-2 (CN02 strain). At the end of the incubation period, the virus was harvested, inactivated with β-propiolactone, concentrated, purified, and finally absorbed onto aluminium hydroxide. The aluminium hydroxide complex was then diluted in a sodium chloride, phosphate-buffered saline, and water solution before being sterilised and filtered ready for injection.




















